|
| MHE / MO / HME Standards Of Care Guide Authored by Harish Hosalkar, MD., MBMS,FCPS,DNB Pediatric Orthopedic Surgeon, Clinical Instructor, University of Pennsylvania School of Medicine, Philadelphia, PA John Dormans, MD. The Children's Hospital of Philadelphia, PA Click Here To View The Standards Of Care Clinical Informational Video Follow Up Companion To This Guide Diagnostic Tools Important features of orthopedic exam: |
It is important to follow each step of the exam during every office assessment of MHE (check the link for
Hereditary Multiple Exostoses: A Current Understanding of Clinical and Genetic Advances)
Hereditary Multiple Exostoses: A Current Understanding of Clinical and Genetic Advances)
Frequency of Follow-up
Note: Your child’s orthopaedist may recommend follow-up at different intervals, sometimes
every 3 months, sometimes a year or more, and can explain why that time frame is indicated.
Characterization of Lesions:
 | Children should be followed up at 6-9 month intervals and sooner if there are any red flags | |
| in terms of sudden increase in size of the bump, pain, tingling, numbness, weakness, visible and progressive limp, limb deformities and length discrepancies | ||
 | It is important to keep a regular follow-up of all cases even after skeletal maturity. Most | |
| patients have increased awareness of all the red flags to be watched for by this time and hence can keep a personal lookout for the same. A thorough exam can be performed by the clinician (including measurements) during the office visit. Radiographs should be repeated only when the bumps are symptomatic or growing. |
Note: Your child’s orthopaedist may recommend follow-up at different intervals, sometimes
every 3 months, sometimes a year or more, and can explain why that time frame is indicated.
Characterization of Lesions:
- Location: Whether the tumor is located in the limb bones, chest wall or ribs, skull, or any
other sites in the body.
 | Pain: Is the lesion associated with pain? If yes: Please view the chronic pain section |
- Intensity: Can be assessed and documented in a lot of ways.
 | On a pain scale of 1 to 10. | |
 | Pain Tracker, all of which can be used as a tool to discuss pain with a child during | |
| an examination. |
- Quality:
 | Do you experience pain on and off (intermittently) throughout the day, or all the | |
| time (constantly)? | ||
 | Does the pain occur at specific times, or with specific activities (ex. Upon waking in | |
| the morning, when walking, etc.) | ||
 | Is pain interfering with your general activities? | |
 | Do you need to use special accommodations at work or school? | |
 | Is pain affecting your mood? | |
 | Do you take medications for pain, or use other treatments (i.e. heat, ice, rest). If | |
| so, are these treatments effective? | ||
 | Tumor pain is often unrelenting, progressive, and often present during the night. | |
 | Is there any shooting pain? (Suggestive of nerve compression) |
- Radiation: Pain radiating to upper or lower extremities or complaints of numbness,
tingling or weakness suggest neurologic compression and requires appropriate workup. 
Onset: 
How was the tumor noticed? 
Was there any history of trauma? 
When did the pain actually start? 
Duration: 
What has been the duration of this new lesion? 
How long have the other lesions been around? 
Progress: Whether the exostosis has remained the same, grown larger, or gotten smaller? 
Associated symptomatology: 
Gait and posture disturbances (especially during follow-up of skull or spinal lesions and in cases of limb-length discrepancies and deformities). 
Any specific history of back pain. If yes, its complete characterization. 
Change in bladder or bowel habits (for evidence of spinal lesions causing cord compression) 
Gynecologic function alterations in girls with pelvic lesions. 
Scoliosis may be associated with spinal lesions and may need to be monitored. 
Night pain if present is a worrisome symptom and needs complete evaluation. Night pain is different than chronic pain in that the pain is not constant and
characteristically wakes the patient from sound sleep. Chronic pain on the other hand
is persistent and would interfere with the sleep pattern by making the patient
restless. Chronic night pain is especially common in MHE cases where the location of
the bump may cause pressure on the exostoses when lying down. Soft beds, air
cushions, lateral positioning and frequent turning may prove to be helpful in these
cases.
Neurologic symptoms may be associated spinal or skull lesions. More commonly, local compression of peripheral nerves due to expanding lesions is encountered in
arms and legs. In addition, several cases of Reflex Sympathetic Dystrophy (RSD)
following MHE surgeries to knees and wrists have been noted. Many patients also
experience other nerve-related symptoms following surgery, including long-lasting
pain and sensitivity around surgical sites long after incisions have healed.
Bursa formation and resulting bursitis may occur as a result of the exostoses and should be recorded. A bursa is a fibrous sac lined with synovial membrane and filled
with synovial fluid and is found. The function of a bursa is to decrease friction
between two surfaces that move in different directions. Therefore, you tend to find
bursae at points where muscles, ligaments, and tendons glide over bones. These
bursae can be either anatomical (present normally) or may be developmental (when
the situation demands). The bursae can be thought of as a zip lock bag with a small
amount of oil and no air inside. In the normal state, this would provide a slippery
surface that would have almost no friction. A problem arises when a bursa becomes
inflamed. It loses its gliding capabilities, and becomes more and more irritated when
it is moved. Bursitis can either result from a repetitive movement or due to
prolonged or excessive pressure.
Diagnostic work-up
Physical examination.
A thorough physical examination of the patient is extremely important in the assessment of MHE
patients.
Radiographs
High quality plain radiographs (X-rays) (anteroposterior and lateral views) should be ordered in
cases presenting with exostoses. Standing postero-anterior and lateral views of the entire spine
on a three-foot cassette should be ordered when spinal lesions are suspected. Special views like
tangential views of the scapula may need to be ordered in some cases. Plain films help to localize
the lesion and give a fairly good idea about its size and dimensions in 2 planes. Also scanograms
help to assess the extent of limb-length discrepancy and its localization. Oblique views of the
spine and special skull views may be ordered in suspected cases.
Advanced Imaging
Radionucleide bone scan (bone scan) is sensitive to pathologies causing increased bone
activities within the skeleton. In combination with SPECT (single photon emission computed
tomography), it gives excellent localization of the area of increased uptake. This is extremely
useful in MHE to locate multiple lesions, especially those that are situated in deeper areas not
amenable to clinical palpation. Further imaging if required, can then be focused. Thallium and
PET (positron emission Tomography) scans are also modalities that can help define the
tumor metastasis especially in those rare cases of malignant degeneration.
Computed Tomography (CAT / CT scan)
CT scans are useful in visualizing the bony architecture particularly as an adjunct to plain
radiographs or bone scans. Thin slice CT cuts may be necessary in small lesions. Two and three-
dimensional reconstructions are possible and add to the information. Rarely the CT may be
combined with the myelogram to effectively delineate the size of the lesion especially for
intraspinal lesions.
Magnetic Resonance Imaging (MRI)
This is an excellent modality for defining the spinal cord, nerve roots, soft tissue structures and
cartilage. Cortical bone is not seen as well as compared with CT. Cartilage caps of the
exostoses and their compression effects on soft-tissues, nerves and adjacent vessels can be
very well delineated. It is a study of choice in suspected cases of malignant transformation. MRI
studies must be reserved for those cases in which clinical signs and symptoms deem them
appropriate. Clinicians must make a point to communicate clinical information and suspected
differential diagnosis to the radiologists.
Other Diagnostic Tools
Ultrasound
May be necessary to diagnose compression of arteries. The principle for ultrasound, or
ultrasonography, is the same as for underwater sonar or echo sounding. An apparatus sends an
ultrasonic wave through the body at a speed of about 1,500 meters per second. At the interface
between two types of tissue, the wave will be refracted or ‘broken up’, and part of the wave will
be reflected back and detected by the apparatus. The rest of the ultrasonic wave continues
deeper into the body, and is reflected as an echo from the surface of tissues lying further inside
the body. How much is reflected depends on the densities of the respective tissues, and thus
the speed of the sound wave as it passes through them. The time taken for the reflected wave
to return indicates how deep the tissue lies within the body. In this way, one obtains a picture of
the relative locations of the tissues in the body, in the same way that one may visualize the
contours of a school of fish with sonar. An ultrasound can help ascertain the status of the blood
flow through the arteries as well and is therefore important for assessment of suspected
compression.
EMG (Electromyography, myogram)
May be necessary in cases of suspected nerve damage
What is EMG
Electromyography (EMG) is a test that measures muscle response to nervous stimulation
(electrical activity within muscle fibers).
How the test is performed
A needle electrode is inserted through the skin into the muscle. The electrical activity detected
by this electrode is displayed on a monitor (and may be heard audibly through a speaker).
Several electrodes may need to be placed at various locations to obtain an accurate study. After
placement of the electrode(s), you may be asked to contract the muscle (for example, by
bending your arm). The presence, size, and shape of the wave form (the action potential)
produced on the monitor provide information about the ability of the muscle to respond when
the nerves are stimulated.
Each muscle fiber that contracts will produce an action potential, and the size of the muscle fiber
affects the rate (frequency) and size (amplitude) of the action potentials. A nerve conduction
velocity test is often done at the same time as an EMG.
Why the test is performed
EMG is most often used when people have symptoms of weakness and examination shows
impaired muscle strength. It can help to differentiate primary muscle conditions from caused
by neurologic disorders. EMG can be used to differentiate between true weakness and reduced
use due to pain or lack of motivation.
Histology
Clinical examination and Imaging findings can help establishing the diagnosis in most cases.
Biopsy should be performed when a malignant change is suspected.
Laboratory evaluation / Genetic Testing (Please also read the MHE Research
Foundations genetics section of the website.)
Test methods:
Sequence analysis of the EXT1 and EXT2 genes are offered as separate tests. Using genomic
DNA obtained from buccal (cheek) swabs or blood (5cc in EDTA), testing of EXT1 proceeds by bi-
directional sequence analysis of all 11 coding exons. The EXT2 gene consists of 15 exons, and
all coding exons (2-15) are sequenced in the analysis.
Test sensitivity:
In patients with MHE, mutations are found in approximately 80% of individuals. Of those in
whom mutations are identified, 70% of the mutations are found in the EXT1 gene and the
remaining 30% in the EXT2 gene. Thus, the method used to screen the EXT1 is expected to
identify approximately 60% of mutations in MHE. In individuals who are found to be negative on
analysis of the EXT1 gene, screening of the EXT2 gene will identify the molecular basis of the
disease in a further 25% of affected individuals. To date, there are no known distinguishing
features within the clinical diagnosis of MHE known to predict which gene is more likely to have a
mutation. Multiple exostoses can be associated with contiguous deletion syndromes, which are
not detected with these methods.
How MHE Can Affect Each Part of the Body
Pick a bone this link will show you all the bones in the body
MHE usually manifests during early childhood more commonly with several knobby, hard,
subcutaneous protuberances near the joints.
The likelihood of involvement of various anatomical sites as observed in a large series is as
follows: Skeleton: The Bones
Anatomical
locationPercentage of
involvementDistal femur 70 Proximal tibia 70 Proximal fibula 30 Proximal Humerus 50 Scapula 40 Ribs 40 Distal radius and
ulna30 Proximal femur 30 Phalanges 30 Distal fibula 25 Distal tibia 20 Bones of the foot 10-25 The Skull
Lesions in the skull, although reported are extremely rare. Mandibular osteochondromas,
typically of the condyle, skull wall lesions and even intracranial lesions have been reported.
Affects of MHE on Skull:
Exostoses can cause problems if they compress or entrap cranial nerves or cause extrinsic
compression on the brain. Effects can range from bumpy external lesions that cause cosmetic
problems, compression of adjacent structures, cranial nerve involvement and even focal
neurological deficits due to compression. Even seizures are likely due to intracranial lesions.
Diagnostic Procedures:
The orthopedist will manually feel for exostoses along the outer table of the skull, check
movements of the mandible and also of the upper cervical spine. The orthopedist will also check
cranial nerve function and perform a thorough neurological evaluation. X-rays or other imaging
tests including CT and MRI may be ordered.
Possible Treatment Options:
Minor lesions on the outer table of the skull that are flat can sometimes be closely observed. 
Bigger lesions on the skull, mandibular lesions causing TM joint instability, and intracranial lesions causing pressure signs may need to be removed by neurosurgical
intervention.
Upper cervical spinal tumors, especially of the atlanto-occipital region may be dealt with by orthopedists. Decompression and or stabilization may be performed as required.
What Parents Should Watch Out For:
Pain. Is your child experiencing pain from exostoses? 
Visible lumps on the face or skull. 
Any symptoms of tingling, numbness, weakness in the hands or legs suggestive of focal deficits. 
Visible lumps on the face or skull. Episodes of seizures or findings of cranial nerve involvement like altered smell, taste, ringing in ears etc. 
Problems in chewing, restricted motion of the jawbone or instability of the mandible. 
Parents can ask dentists and orthodontists to be on the lookout for signs suggestive of jawbone instability or joint involvement during their office visits especially in symptomatic
cases.
Spine
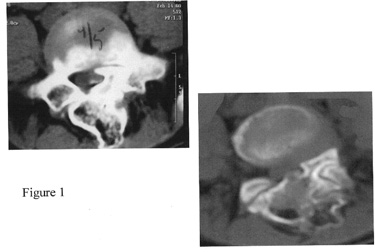
The spine extends from the base of the skull to the tailbone. Spinal exostoses are rare (Figure
1). Spinal cord impingement is also a rare, but documented, complication of MHE. Cervical,
thoracic or lumbar region can be affected. Scoliosis secondary to spinal osteochondromas and
instability has been reported.
 Affects of MHE on the Spine: more views of the spine can be seen on the MHE
Affects of MHE on the Spine: more views of the spine can be seen on the MHE
Research Foundation image gallery
This section of the body is not commonly involved with MHE. Involvement of isolated vertebrae
has been noted. Affects can range from instability to neural root or cord compression that can
manifest as tingling, numbness or weakness in the involved roots or even major neurological
deficits like paraparesis or quadriparesis in untreated cases. Rarely compression effects in the
form of dysphagia, intestinal obstruction or urinary symptoms may occur.
Diagnostic Procedures:
With any of the red flags mentioned earlier, the orthopedist will perform a thorough spinal and
neurological evaluation. Plain x-rays of the spine and if required, advanced imaging may be
performed. The presences and extent of the lesion are best delineated with CT, while MRI of the
spinal cord demonstrates the area of spinal cord impingement. In rare cases of peripheral nerve
compression electromyography may be performed to check status of the nerve.
Possible Treatment Options:
Minor lesions not causing compressive symptoms or neurologic manifestations may be kept under close observation. 
Progressive scoliosis and spinal instability may need to be treated with surgical stabilization involving spinal fusion.
What Parents Should Watch Out For:
Any red flags in terms of tingling, numbness, weakness, night pain or bladder and bowel changes and get them evaluated. 
Any deformity in the spine or evidence of shoulder or pelvic imbalance. 
Gait or posture disturbances. Remember that gait and posture disturbances can be caused by hip or leg exostoses as well (due to either limb-length discrepancy or deformity)
and do not necessarily mean tumors in the spine. In any case evaluation by a clinician is
important.
Ribs and Sternum
Affects of MHE on the ribs and sternum:
The typically flat bones of the ribs are prone to effects of MHE, with approximately 40% of MHE
patients having rib involvement. Prominent chest wall lesions are common although intrathoracic
lesions including rare presentations like spontaneous hemothorax (build-up of blood and fluid
in the chest cavity) as a result of rib exostoses have been described. Typically, these lesions
create issues of cosmesis due to their obvious visibility. Other symptoms may include shortness
of breath and other breathing difficulties, pain when taking a deep breath, when walking or
exercising, or pain from exostoses “catching”.
Diagnostic Procedures:
The orthopedist will probably manually feel for exostoses along the chest wall and the ribcage.
Size and extent of the lesions are noted. A thorough pulmonary evaluation is warranted in all
cases when specific symptoms of cough, chest pain or breathing problems are encountered. X-
rays or other imaging tests may be ordered.
Possible Treatment Options:
Pulmonary: when there are severe breathing difficulties with increasing chest pain.
Minor bumps can sometimes be kept under observation. 
Cosmetic problems, rapid increase in size, large size, and signs of compression are some indications for early removal. 
Consult may be required with specialists:
Thoracic surgeons: when intrathoracic (within the chest wall) exostoses may need to be excised.
What Parents Should Watch Out For:
Breathing difficulties, shortness of breath. 
Pain when taking deep breath.
Shoulder girdle
The scapula is a fairly common site (40%) of involvement in MHE. The lesions may be located onthe anterior or posterior aspect of the scapula. Anterior scapular lesions may lead to discomfort
during scapulothoracic motion. Winging of the scapula due to exostoses has been described.
Clavicle (collar bone) involvement has also been described (5% cases).
What is winging?
The scapula (also known as shoulder blade) is a triangular flat bone that is located in the upper
back and takes part in forming the shoulder joint. The scapula usually lies flat on the chest wall
without any prominence. Winging of the scapula is a phenomenon when a part of the scapula
including the inferior angle becomes prominent either at rest or during movements.
The two most common causes for this are
Exostosis on the inner (chest wall) aspect of the scapula. 
Damage to the nerve (long thoracic) causing weakness or paralysis of muscles (serratus anterior) attached to the scapula.
Diagnostic Procedures:
The orthopedist will probably manually feel for exostoses along the outer aspect of the shoulder
blade. Some limited areas of the inner aspect are amenable to clinical examination. Range and
feel of the scapulothoracic motion is helpful in clinical assessment. It is important to check
individual groups of scapular muscles to rule out nerve compression leading to winging of
scapula. X-rays (including special tangential views of the scapula) or other imaging tests may be
ordered.
Possible Treatment Options:
Both outer aspect lesions and inner ones may need excision in symptomatic cases. Smaller lesions on outer aspect amenable to clinical palpation may be observed with regular clinical
follow-up.
What Parents Should Watch Out For:
Crunching or crackling sound when moving that area. 
Pain. 
Tingling, numbness.
Arms
Upper Arm (X-rays) (Humerus) 
Elbow 
Forearm (Radius and Ulna) 
Wrists The arm bone is called the humerus while the forearm bones are the radius (curved bone) and
the ulna (straighter bone of the two). To view more x-rays please view the MHE Research
Foundations image galery
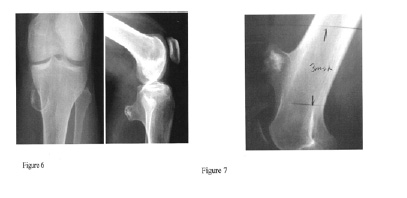
Osteochondromas of the arm are often readily felt but rarely cause neurologic dysfunction.
(Figure 2). Osteochondromas of the upper extremities frequently cause forearm deformities.
The prevalence of such deformities has been reported to be as high as 40-60%.
Disproportionate ulnar shortening with relative radial overgrowth has been frequently described
and may result in radial bowing. Subluxation or dislocation of the radial head is well-described
sequelae in the context of these deformities.
The length of forearm bones inversely correlates with the size of the exostoses. Thus, the
larger the exostoses and the greater the number of exostoses, the shorter the involved bone.
Moreover, lesions with sessile rather than pedunculated morphology have been associated with
more significant shortening and deformity. Thus, the skeletal growth disturbance observed in
MHE is a local effect of benign growth. Exostoses in the forearm are known to involve both the
radius and the ulna. Since movements of the forearm (pronation and supination) are
dependant on the radius moving in an arc of motion around the ulna, mobility may be restricted
depending upon the severity of presentation. Also the lower end radius exostoses can lead to
compression of the median nerve (in a closed space at the level of the wrist called the carpal
tunnel) and present with weakness, tingling and numbness in the hand. Exostoses in the carpal
bones can seriously hamper the wrist motion and cause pain.
Complete dislocation of the radial head is a serious progression of forearm deformity and can
result in pain, instability, and decreased motion at the elbow. Surgical intervention should be
considered to prevent this from occurring. When symptomatic, this can be treated in older
patients with resection of the radial head.
Diagnostic Procedures:
The orthopedist will clinically feel for exostoses along the arm, elbow and forearm, and check
range of motion (“ROM”) by moving the arm in different directions. The orthopedist will also
check measurements on each arm and forearm to see if there is a difference. X-rays or other
imaging tests may be ordered.
Possible Treatment Options:
Indications for surgical treatment include painful lesions, an increasing radial articular angle, progressive ulnar shortening, excessive carpal slip, loss of pronation, and increased radial
bowing with subluxation or dislocation of the radial head Minor lesions can sometimes be
observed with careful follow up.
Bowing and some length discrepancies and be treated with a surgical procedure called “stapling,” where surgical staples are inserted into the growth plate of the bone growing
faster than the other. This will hopefully give the slower growing bone the chance to “catch
up” and the forearm will straighten over time.
Limb Lengthening with a fixator. 
Resection of the radial head. 
Excision of exostoses. 
Osteotomy 
Epiphysiodesis 
Non-surgical measures for treatment of soft-tissue compression, irritation or inflammation (anti-inflammatories, heat, rest, etc.)Adaptive devices to aid those with shortened
forearms, such as grippers, long-handled sock aides, etc.
What Parents Should Watch Out For:
Any red flags in terms of sudden increase in size of swelling, pain, nerve compression, tingling, numbness, or weakness. 
Possibility of exostoses irritating or catching on overlying tissue, such as muscles, tendons, ligaments, or compressing nerves. 
Loss of range of motion 
Pain 
Difficulty and/or pain when raising arm(s), lifting, carrying
Please also refer to the MHE Research Foundations fixator information guide. Their are alsomore links located in the Green Table at the bottom of the orthopaedic page and in the tool bar
Hands and Fingers
Hand involvement in MHE is common. Fogel et al. observed metacarpal involvement and
phalangeal involvement in 69% and 68%, respectively, in their series of 51 patients. In their
series of 63 patients, Cates and Burgess found that patients with MHE fall into two groups:
those with no hand involvement and those with substantial hand involvement averaging 11.6
lesions per hand. They documented involvement of the ulnar metacarpals and proximal
phalanges most commonly with the thumb and distal phalanges being affected less frequently.
While exostoses of the hand resulted in shortening of the metacarpals and phalanges,
brachydactyly was also observed in the absence of exostoses.
Diagnostic Procedures:
The orthopedist will manually feel for exostoses in the hands and check range of motion
(“ROM”) in different directions. X-rays or other imaging tests may be ordered.
Possible Treatment Options:
Isolated lesions growing rapidly, or interfering with the smooth motion of tendons or joint motion may need to be excised. Multiple surgeries for small, insignificant lesions is usually
not advocate.
Occupational therapy, physical therapy. 
Use of pencil grips, laptop computers, and other adaptive devices.
What Parents Should Watch Out For:
Complaints of pain when writing. 
Some children will not complain of pain, but will have poor penmanship, write slowly, avoid writing, etc. Parents should also observe how the child holds writing and eating utensils. 
Difficulty in rotating hand(s),
Pelvic Girdle (Hips and Pelvis) Osteochondromas of the proximal femur (Figure 3) may lead to progressive hip dysplasia. There have
Osteochondromas of the proximal femur (Figure 3) may lead to progressive hip dysplasia. There have
been reported cases of acetabular dysplasia with subluxation of the hip in patients with MHE. This results
from exostoses located within or about the acetabulum that may interfere with normal articulation.
 Pelvic lesions (Figures 4 and 5) may be found on both the inner as well as outer aspect of the
Pelvic lesions (Figures 4 and 5) may be found on both the inner as well as outer aspect of the
pelvic blades. Large lesions may cause signs of compression, both vascular and neurological. There
have also been reports of exostoses interfering with normal pregnancy and leading to a higher
rate of Cesarean sections. To view more x-rays please view the MHE Research Foundations
image galery
Diagnostic Procedures:
Manual palpation is sometimes very difficult in these deep lesions. The orthopedist will check range
of motion (“ROM”) by manipulating (moving) the leg in different directions. The orthopedist will
also check measurements on each leg to see if there is a difference in limb lengths. X-rays or other
imaging tests may be ordered.
Possible Treatment Options:
Minor length discrepancies can sometimes be effectively treated with the use of orthotics (specially made shoes or lifts that will equalize leg length). 
Bowing and some limb length discrepancies can be treated with a surgical procedure called “stapling,” where surgical staples are inserted into the growth plate of the leg bone growing
faster than the other. This will hopefully give the slower growing bone the chance to “catch
up” and the limb will straighten over time.
Limb Lengthening with a Fixator. Please see the lower limb & forearm, use of fixators guide located in the website tool bar above 
Pelvic lesions of concern may need to be surgically excised. 
Osteotomies. 
Hip replacement.
What Parents Should Watch Out For:
Limping 
Pain in hips, back, legs. 
Pain, discomfort, difficulty in sitting. 
Inability to sit “tailor” style. The position known as Indian or tailor style involves both feet bent inwards and under the body, crossing each other at the ankle. 
Stiffness in hips and/or legs after sitting. 
Pain and fatigue from walking.
Legs and Knees
Femur 
Knees 
Lower Leg (Tibia and Fibula) 

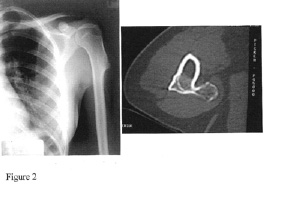
 Genu Valgum or Knock-knee deformities are found in 8-33% of patients with MHE. Genu
Genu Valgum or Knock-knee deformities are found in 8-33% of patients with MHE. Genu
valgum is defined as a mechanical malalignment of the lower limb when the knees knock against
each other and the legs are pointed away from the body. Although distal femoral involvement is
common, the majority of cases of angular limb deformities are due mostly to lesions of the tibia
and fibula (Figures 8,9 & 10), which occur in 70-98% and 30-97% of cases, respectively. The
fibula has been found by Nawata et al. to be shortened disproportionately as compared to the
tibia, and this is likely responsible for the consistent valgus direction of the deformity. Genu
varum or Bowlegs may also occur in some cases. This is defined as a mechanical malalignment of
the lower limb when the knees drift away from the body and the legs are bowed and close
together.
 To view more x-rays please view the MHE Research Foundations image galery
To view more x-rays please view the MHE Research Foundations image galery
Diagnostic Procedures:
The orthopedist will probably manually feel for exostoses along the leg, and check range of
motion (“ROM”) by manipulating (moving) the leg in different directions. The orthopedist will
also check measurements on each leg to see if there is a difference. X-rays or other imaging
tests may be ordered.
Possible Treatment Options:
Minor length discrepancies can sometimes be effectively treated with the use of orthotics (specially made shoes or lifts that will equalize leg length). 
Bowing and some limb length discrepancies and be treated with a surgical procedure called “stapling,” where surgical staples are inserted into the growth plate of the leg bone
growing faster than the other. This will hopefully give the slower growing bone the chance
to “catch up” and the limb will straighten over time.
Limb Lengthening with a Fixator. Please see the lower limb & forearm fixator guide and other links located in the website tool bar above. 
Excision of exostoses 
Osteotomy
What Parents Should Watch Out For:
Any red flags in terms of sudden increase in size of swelling, pain, nerve compression, tingling, numbness, or weakness. 
Possibility of exostoses irritating or catching on overlying tissue, such as muscles, tendons, ligaments, or compressing nerves. 
Leg cramps, bluish color, difference in skin temperature may indicate compression of a artery (most often the popliteal artery, located behind the knee). 
Compression of the peroneal nerve, which runs along the outside of the leg, can cause a condition known as “drop foot”, in which the foot cannot voluntarily be flexed up.
Compression can be caused by exostoses growth, or as a complication of surgery.
Limping, pain when walking. 
Bowing of leg(s) 
Exostoses on inside of legs bumping into each other. 
Exostoses interfering with normal movements, either by blocking movement or by causing pain (bending, sitting, walking up or down stairs). 
Pain and fatigue when walking. 
Gait problems (awkwardness, limping, slow movements, etc.)
Ankles
Valgus deformity of the ankle is also common in patients with MHE and is observed in 45-54% ofpatients in most series. This valgus deformity can be attributed to multiple factors including
shortening of the fibula relative to the tibia. A resulting obliquity of the distal tibial epiphysis
and medial subluxation of the talus can also be associated with this deformity, while
developmental obliquity of the superior talar articular surface may provide partial compensation.
Diagnostic Procedures:
The orthopaedist will probably manually feel for exostoses along the leg, and check range of
motion (“ROM”) by manipulating (moving) the leg in different directions. The orthopaedist will
also check measurements on each leg to see if there is a difference. X-rays or other imaging
tests may be ordered.
Possible Treatment Options:
Minor length discrepancies can sometimes be effectively treated with the use of orthotics (specially made shoes or lifts that will equalize leg length). 
Bowing and some limb length discrepancies and be treated with a surgical procedure called “stapling,” where surgical staples are inserted into the growth plate of the leg bone
growing faster than the other. This will hopefully give the slower growing bone the chance
to “catch up” and the limb will straighten over time.
In more advanced cases, excision of exostoses with early medial hemiepiphyseal stapling of the tibia in conjuction with exostosis excision can correct a valgus deformity at the ankle of
15° or greater associated with limited shortening of the fibula.
Fibular lengthening has been used effectively for severe valgus deformity with more significant fibular shortening, (i.e. when the distal fibular physis is located proximal to the
distal tibial physis).
Supramalleolar osteotomy of the tibia has also been used effectively to treat severe valgus ankle deformity. 
Growth of exostoses can also result in tibiofibular diastasis that can be treated with early excision of the lesions.
What Parents Should Watch Out For:
Limping, pain when walking. 
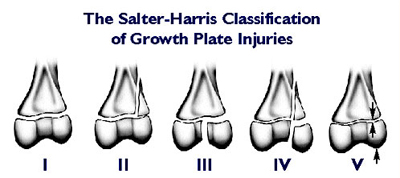
Recurrent falls and instability while walking on uneven surfaces. Parents should be aware that falls could result in what are known as Salter-Harris Fractures / (Growth plate
fractures) this has been seen to occur in children with MHE / MO / HME. If your child falls
and the pain is occurring around the growth plate area of the joint, this should be checked
by your orthopaedic doctor. As these type of fractures can also lead to bone deformity.Disclaimer: While many find the information useful, it is in no way a substitute for professional
medical care.The information provided here is for educational and informational purposes only. This
website does not engage in the practice of medicine. In all cases we recommend that you consult your
own physician regarding any course of treatment or medicine.
Email the webmaster: webmaster@mheresearchfoundation.org
Materials on this website are protected by copyright
Copyright © 2008 The MHE Research FoundationThis file will print 17 pages
Feet and Toes
Osteochondromas may occur in the tarsal and carpal bones, however they are often less
apparent. Relative shortening of the metatarsals, metacarpals, and phalanges may be noted.
Diagnostic Procedures:
Plain radiographs are probably more useful in defining the extent of involvement of the small
bones of the feet in MHE. Other imaging studies may be ordered as and when required.
Possible Treatment Options:
Large bumps can be surgically excised when symptomatic. 
Deformities of the foot (like hallux valgus) may be corrected by stapling of the growing epiphysis in younger children or by surgical osteotomy in older patients.
What Parents Should Watch Out For:
Compression of the peroneal nerve, which runs along the outside of the leg, can cause a condition known as “drop foot”, in which the foot cannot voluntarily be flexed up.
Compression can be caused by exostoses growth, or as a complication of surgery.
In general
“What Parents Should Watch Out For”
If your child is limping, check to see if it is due to an injury, or is something that is occurring and continuing without obvious reason. Limping may signal a limb length
discrepancy or other problem.
Bowing of one or both legs. 
Mobility problems. Is your child experiencing pain when walking or running? 
Pain. Is your child experiencing pain from exostoses that bump each other? Is your child experiencing pain during certain activities, or pain at night. If so, keep a pain diary. 
Any red flags in terms of sudden increase in size of swelling, pain, nerve compression, tingling, numbness, or weakness
What Adults Should Be Aware Of:
Sudden growth in an existing exostosis and pain can be symptomatic of a malignant transformation. It is smart to check out any changes with your orthopaedist. However,
it is important to remember that chondrosarcoma is rare.
Years of wear and tear on joints can result in chronic pain. There is also the possibility of exostoses irritating or catching on overlying tissue, such as muscles, tendons, ligaments,
or compressing nerves. Possible Treatment Options for these common problems, include
pain medications, physical therapy (including stretching, strengthening and modalities),
heat, rest, bracing (supportive orthosis acting as load sharing devices) etc.
Glossary of terms and procedures:
Synonyms of multiple exostoses: A number of synonyms have been used for this disorder
including osteochondromatosis, multiple hereditary osteochondromata, multiple congenital
osteochondromata, diaphyseal aclasis, chondral osteogenic dysplasia of direction, chondral
osteoma, deforming chondrodysplasia, dyschondroplasia, exostosing disease, exostotic
dysplasia, hereditary deforming chondrodysplasia, multiple osteomatoses, and osteogenic
disease.
Anterior: Situated in the front; forward part of an organ or limb
Ball and socket joints: Movable (synovial) joints, such as hips and shoulders, that allow a
wide range of movement.
Bilateral: having two sides or pertaining to both sides.
Biopsy: Take a piece of the lesion to study the histological characteristics.
Cartilage: Form of connective tissue, more elastic than bone, which makes up parts of the
skeleton and covers joint surfaces of bones.
Coxa-valga: When the thighbones are drawn farther apart from the midline due to an increase
in the neck-shaft angle of the femur.
Coxa-vara: When the thighbones are drawn closer to the midline due to a decrease in the neck-
shaft angle of the femur.
Dislocation: When the normal articulating joint surfaces have lost total contact.
Distal: Away from the midline or the beginning of a body structure (the distal end of the
humerus forms part of the elbow).
Epiphysiodesis: To surgically stop the growth of the growing end of the bone either
temporarily or permanently.
Excision: To surgically remove the lesion.
Genu-valgum: Knock-knees.
Genu-varum: Bowlegs.
Hinge joints: movable joints, such as knees and elbows, that allow movement in one direction.
Limb-lengthening: Process of increasing the length of bones using one of the various devices.
Also view
lower limb & forearm fixator guide and other links located in the website tool bar above.
LLD: Limb-length discrepancy- difference in limb lengths.
Medial: Pertaining to the middle or toward the midline.
MHE: An autosomal-dominant disorder manifested by multiple osteochondromas and frequently
associated with characteristic skeletal deformities.
Osteochondromas: Cartilage capped tumors found commonly at rapidly growing ends of bones.
Osteotomy: The surgical division or sectioning of a bone.
Pedunculated: Lesion with a stalk connecting it to the main bone.
Posterior: Situated in the back; back part of an organ or limb
Proximal: Near the midline or beginning of a body structure (the proximal end of the humerus
forms part of the shoulder).
Sessile: Lesion without a stalk connecting it to the main bone.
Stapling: Process of insertion of a mechanical device (staple) following surgical intervention.
Subluxation: When the joint surfaces are still facing each other but not totally in contact.


Graphic provided by http://www.niams.nih.gov/Health_Info/Growth_Plate_Injuries/graphics/growth-plate.jpg